Wasp Barcode Technologies: The Barcode Solution People
FMD, S4S, and ADS: The Future of Medicinal Barcodes

9 February 2019 will bring a new level of safety into medicinal practices. On that date, the EU
Falsified Medicines Directive (FMD) will go into effect.
Under the FMD,
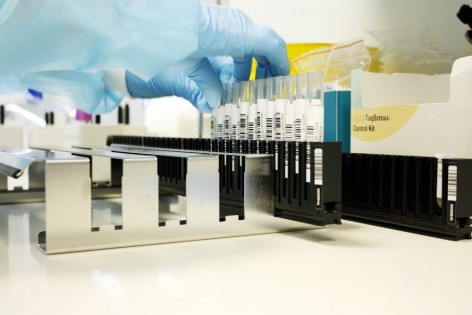
all prescription medicine packs will be required to possess a unique 2D barcode that will be held in a national database. Pharmacies will be required to scan the code on each pack to confirm that particular pack is registered prior to dispense to patients. Also required will be a tamper-evident seal that will be checked just prior to delivery.
[Tweet "Also required will be a tamper-evident seal that will be checked just prior to delivery."]
The hope behind the FMD is that it will protect patients by making it more difficult for
counterfeit medications from entering the supply chain. It also allows – more to point, it
requires – everyone along this chain to verify the authenticity and security of the product before it reaches its literal consumer.
FMD can be seen as an evolution in the way
barcode-based inventory management can help increase accuracy, efficiency, and accountability to your asset handling and assignments. For even further increased accountability, you can easily
print your facility’s codes in-house. Affix them to medications, patient charts, identification bands, hospital equipment. Use handheld scanners or scanner apps to scan these codes at each patient encounter to help ensure the proper patient receives the appropriate care.
Staff can reduce the time spent on comparison of chart to doctor’s orders to file medications. Simply scan the code, access the files on the hospital’s system, and confirm with a secondary scan. Administer treatment.
The creation of individalised barcodes for each patient is also a step toward a
paper-free existence sought by the NHS before 2020. Aside from a reduction in errors, the department hopes to save between £500,000 to £1 million per healthcare trust to then invest in more personnel.

Barcodes assigned to medications can also be tagged to alert for restock whenever supplies dip below a certain level. The inclusion of medication expiration dates can help save an estimated hour of time otherwise spent in the search for something, be it an out-of-date stock or an out-of-stock one.
An additional perk of barcoded supplies: Coded tools and artificial joints can easily be identified in the
event of a recall due to fault or failure. These codes can (and should) be scanned
at least twice prior to surgery: Once when retrieve for the procedure and once again prior to implantation. (Note: This precludes to scans upon arrival to the facility, which should be a given).
These scans become a part of the patient record which becomes part of the facility’s database. Should a recall come, the code identity can be search for and related hits can then be contacted for corrective surgery or whatever other options might be available. Records will also show which staff member provided treatment along with the date and time in the event of a mishap.
The Department of Health projects a
savings of up to £1billion over seven years through nationwide application of what it calls “Scan4Safety.”
Picture the potential difference of Scan4Safety in 2010 when PIP breast implants faced a massive recall with almost
50,000 British women the recipients of said devices. The implants contained industrial grade silicone, not medical grade, and carried an rupture rate double that of other implants.
Problems arose because some surgery providers that performed the implantations went out of business. As such, these records no longer existed and some recipients could not be traced.
With Scan4Safety, implants and devices will be barcoded with the ability for monitoring to compare durability or failure rates when times comes for inspection and replacement. The
six pilot facilities involved already report a measurable reduction in unnecessary waste and improvement medicinal management. This time can better go toward improved patient care and education.
Automation is another case for barcode identification of medicines. Look at the
King’s Lynn hospital pharmacy: The facility will soon implement a £600,000 Automated Dispensing System that will choose, dispense, and label outgoing medications in under seven seconds! The plan will, in theory, reduce dispensing times (to help patients receive their medications quickly) and to reduce the workload experienced by staff.
Medications will be stored in the ADS’s body and selected by – what else? – the appropriate barcode. It will then travel along a conveyor belt where it will travel, properly readied, to head toward its final destination.
The level of automation is also expected to help increase the effectiveness of stock use with code access and expiration information on hand.
Barcodes alone do not, of course, a fool-proof system make and errors can still occur. Errors and
accidents can lead to severe consequences, especially when it comes to medication mistakes. The wrong medications given to the wrong patient may lead to an allergic reaction or conflicts between prescriptions with potentially fatal side effects. While barcode scanning drastically reduces the potential for these occurrences, mistakes happen.
In
March 2013, a father of two receive a prescription from his local pharmacy. While the label read exactly as it should, the box itself contained a completely different substance and almost cost the man his life.
Such a mistake
could still happen with in-house barcode printing without proper due diligence, but the chances remain considerably lower when one must scan the master code to bring up these medications in the database
and the code on the medication itself.
 9 February 2019 will bring a new level of safety into medicinal practices. On that date, the EU
9 February 2019 will bring a new level of safety into medicinal practices. On that date, the EU  Barcodes assigned to medications can also be tagged to alert for restock whenever supplies dip below a certain level. The inclusion of medication expiration dates can help save an estimated hour of time otherwise spent in the search for something, be it an out-of-date stock or an out-of-stock one.
An additional perk of barcoded supplies: Coded tools and artificial joints can easily be identified in the
Barcodes assigned to medications can also be tagged to alert for restock whenever supplies dip below a certain level. The inclusion of medication expiration dates can help save an estimated hour of time otherwise spent in the search for something, be it an out-of-date stock or an out-of-stock one.
An additional perk of barcoded supplies: Coded tools and artificial joints can easily be identified in the 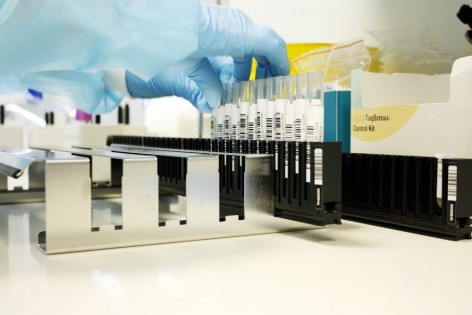 The Department of Health projects a
The Department of Health projects a

